Dental crowns are one of the most common solutions for restoring damaged or weakened teeth. A skilled dental team can help you determine whether a crown is the right option for your situation. This post breaks down what dental crowns actually are, why dentists use them, and the different materials available. We’ll also walk through the procedure step by step and cover the benefits you can expect. Knowing how to care for your crown will help it last for years.
Definition of Dental Crown
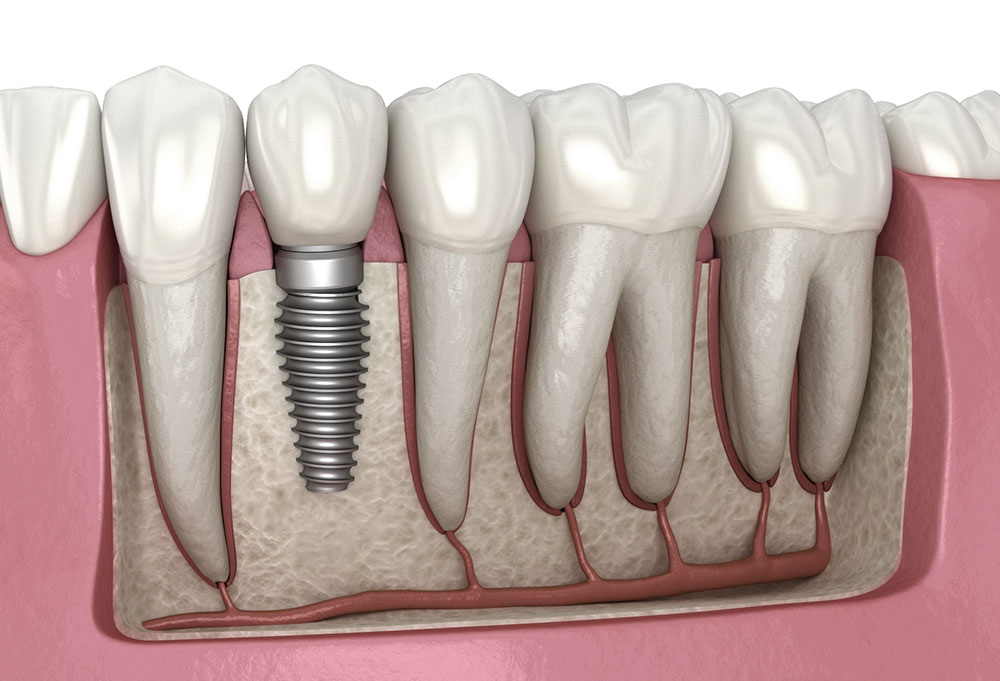
A dental crown is basically a tooth-shaped cap that fits over a damaged or weak tooth. It restores the tooth’s shape, size, and strength while making it look better, too. Crowns are commonly used after significant decay, large fillings, or root canal treatments. These caps can be made from materials such as porcelain, metal, or a combination of both, depending on the patient’s needs. The process involves reshaping the tooth for a proper fit, taking impressions for customization, and then cementing the crown securely in place. Dental crowns play a big role in preserving both the structure and appearance of a compromised tooth.
Purpose of Dental Crowns
The main goal of a dental crown is to protect and support a weakened or damaged tooth. When a tooth is badly decayed, cracked, or structurally compromised, a crown can bring back its strength and function. Crowns are custom-made caps that cover the entire visible part of a tooth above the gum line, completely wrapping it. By fitting snugly over the tooth, crowns act as a shield, preventing further damage and protecting the underlying tooth structure. This barrier also keeps the tooth aligned properly in your mouth, so your bite and chewing function stay on point. Dental crowns help maintain oral health by protecting compromised teeth and stopping potential problems before they start.
Types of Dental Crown Materials
Dentists use several types of crown materials to fit different patient needs and preferences. The most common options include metal, porcelain-fused-to-metal, all-ceramic, and zirconia crowns. Metal crowns (such as gold or silver alloys) are durable and require less tooth removal. Porcelain-fused-to-metal crowns look natural thanks to their tooth-colored exteriors. All-ceramic crowns are popular for their great appearance, making them a solid choice for front teeth. Zirconia crowns are known for their strength and are often used on back teeth. Each material has its pros and cons, so talking to your dentist helps determine the best fit for your specific situation.
Procedure for Getting a Dental Crown
Getting a dental crown involves a few straightforward steps. The dentist starts by reshaping the tooth so the crown can fit over it properly. Then they take impressions of the tooth and the surrounding teeth to ensure the crown fits perfectly. These impressions guide the creation of your custom crown. While the permanent crown is being made, the dentist places a temporary crown to protect the prepared tooth. Once the permanent crown is ready, the temporary one comes off, and the new crown gets cemented in place. The dentist makes any needed adjustments to get the fit and bite alignment right. Regular check-ups help monitor the condition of the crown and your overall oral health.
Benefits of Dental Crowns
Dental crowns offer solid protection and support for weak or damaged teeth. They restore strength and function to teeth that have undergone severe decay or damage. By covering the entire visible portion of the tooth, crowns prevent further breakdown and potential fractures. They also maintain proper alignment and bite structure, reducing the risk of tooth shifting over time. On top of that, dental crowns can make a tooth look better, improving your smile’s appearance. With proper care, crowns can last many years, making them a durable, long-term solution for dental problems. The benefits add up to better oral health for anyone dealing with tooth restoration.
Maintenance and Care for Dental Crowns
Taking care of your dental crown helps it last longer. Follow these three guidelines to get the most out of your crown:
- Oral Hygiene: Brush and floss regularly to prevent plaque buildup around the crown area.
- Regular Dental Check-ups: Schedule routine visits so your dentist can check on your crown’s condition and catch any issues early.
- Avoid Hard Foods: Stay away from biting on hard objects or foods like ice and hard candies to prevent damage or loosening.
Related Topics: